Fluid balance hesi case study – The topic of fluid balance takes center stage in this HESI case study. We delve into the intricate details of fluid management, exploring the patient’s symptoms, assessment findings, and the comprehensive interventions employed to restore fluid balance.
Our journey begins with a thorough examination of the patient’s vital signs, physical examination findings, and laboratory results. These assessments provide valuable insights into the patient’s fluid status and guide our diagnostic and management decisions.
Case Overview

The patient presents with complaints of fatigue, weakness, and dizziness. Her medical history includes a recent episode of gastroenteritis, during which she experienced significant vomiting and diarrhea. Based on these symptoms and history, a fluid balance issue is suspected.
Rationale for Suspecting a Fluid Balance Issue
The patient’s symptoms of fatigue, weakness, and dizziness are all consistent with dehydration. Dehydration occurs when the body loses more fluids than it takes in, resulting in a decrease in the body’s total fluid volume. This can lead to a decrease in blood pressure, which can cause dizziness and fainting.
Additionally, dehydration can lead to an electrolyte imbalance, which can cause muscle weakness and fatigue.The patient’s recent episode of gastroenteritis is also a risk factor for dehydration. Vomiting and diarrhea can both lead to significant fluid loss, which can quickly lead to dehydration if not replaced.
Assessment: Fluid Balance Hesi Case Study
The assessment of fluid balance involves evaluating vital signs, performing a physical examination, and reviewing laboratory and diagnostic tests.
Vital Signs
Vital signs provide essential information about the patient’s overall health and can indicate fluid imbalances.
| Vital Sign | Patient’s Value | Significance |
|---|---|---|
| Blood Pressure | 100/60 mmHg | Hypotension, indicating hypovolemia (dehydration) |
| Heart Rate | 110 bpm | Tachycardia, indicating compensatory response to hypovolemia |
| Respiratory Rate | 24 breaths/min | Tachypnea, indicating compensatory response to hypovolemia |
| Temperature | 38.5°C (101.3°F) | Fever, indicating possible infection or dehydration |
Physical Examination
Physical examination findings can provide clues about fluid status.
The fluid balance HESI case study delves into the complexities of maintaining proper hydration. To delve deeper into art history, check out ap art history 250 flashcards . Returning to our case study, we can explore how fluid imbalances can affect electrolyte levels and overall health.
- Skin turgor:Poor skin turgor, indicating dehydration
- Mucous membranes:Dry mucous membranes, indicating dehydration
- Edema:Absent edema, indicating hypovolemia
- Capillary refill time:Prolonged capillary refill time, indicating hypovolemia
Laboratory and Diagnostic Tests
Laboratory and diagnostic tests can confirm fluid imbalances and assess their severity.
- Serum sodium:142 mEq/L, indicating hyponatremia (dilution of sodium)
- Serum potassium:3.5 mEq/L, indicating hypokalemia (depletion of potassium)
- Hematocrit:45%, indicating hemoconcentration (increased red blood cell count due to dehydration)
- Urine specific gravity:1.005, indicating dilute urine (indicating fluid overload)
Diagnosis and Differential Diagnosis
After reviewing the patient’s symptoms, physical exam findings, and laboratory results, the primary diagnosis is dehydration.
The patient presents with signs and symptoms characteristic of dehydration, including decreased skin turgor, dry mucous membranes, and a weak pulse. The laboratory results reveal elevated serum sodium and decreased urine output, further supporting the diagnosis of dehydration.
Differential Diagnoses
Several other conditions can cause similar symptoms to dehydration, including:
- Addison’s disease:This condition causes the body to produce insufficient cortisol, which can lead to dehydration and electrolyte imbalances.
- Diabetes insipidus:This condition causes the body to produce insufficient antidiuretic hormone (ADH), which can lead to excessive urination and dehydration.
- Hyperthyroidism:This condition can cause increased metabolism and fluid loss, leading to dehydration.
These differential diagnoses were ruled out based on the patient’s history, physical exam findings, and laboratory results. For example, the patient does not have a history of Addison’s disease or diabetes insipidus, and their thyroid function tests are normal.
Management
The management of fluid balance involves a comprehensive approach to ensure adequate fluid intake, electrolyte balance, and appropriate medication administration.
To achieve these goals, several interventions are implemented, including fluid management, electrolyte management, and medication administration.
Fluid Management
Fluid management involves monitoring and maintaining the patient’s fluid intake and output to prevent dehydration or fluid overload.
- The patient’s fluid intake is closely monitored and recorded, including oral intake, intravenous fluids, and other sources of hydration.
- Fluid output is also measured and recorded, including urine output, stool output, and insensible losses (e.g., through sweat and respiration).
- Based on the patient’s fluid balance assessment, interventions are implemented to adjust fluid intake and output as needed.
- For example, if the patient is dehydrated, intravenous fluids may be administered to replenish fluids and electrolytes.
- Conversely, if the patient is experiencing fluid overload, fluid restriction and diuretics may be used to reduce fluid retention.
Electrolyte Management, Fluid balance hesi case study
Electrolyte management involves monitoring and maintaining the patient’s electrolyte levels to prevent electrolyte imbalances.
Electrolytes are essential minerals that play crucial roles in various bodily functions, such as nerve conduction, muscle contraction, and fluid balance.
The patient’s electrolyte levels are measured through blood tests, and interventions are implemented to correct any imbalances.
| Electrolyte | Normal Range | Implications of Abnormalities |
|---|---|---|
| Sodium | 135-145 mEq/L | Hyponatremia (low sodium): can cause seizures, coma Hypernatremia (high sodium): can cause dehydration, confusion |
| Potassium | 3.5-5.0 mEq/L | Hypokalemia (low potassium): can cause muscle weakness, arrhythmias Hyperkalemia (high potassium): can cause cardiac arrest |
| Chloride | 96-106 mEq/L | Hypochloremia (low chloride): can cause metabolic alkalosis Hyperchloremia (high chloride): can cause metabolic acidosis |
| Bicarbonate | 22-29 mEq/L | Metabolic acidosis (low bicarbonate): can cause coma Metabolic alkalosis (high bicarbonate): can cause seizures |
| Calcium | 8.5-10.2 mg/dL | Hypocalcemia (low calcium): can cause muscle cramps, seizures Hypercalcemia (high calcium): can cause kidney stones, confusion |
| Magnesium | 1.5-2.5 mEq/L | Hypomagnesemia (low magnesium): can cause muscle weakness, seizures Hypermagnesemia (high magnesium): can cause respiratory depression |
| Phosphorus | 2.5-4.5 mg/dL | Hypophosphatemia (low phosphorus): can cause muscle weakness, bone pain Hyperphosphatemia (high phosphorus): can cause kidney stones, skin itching |
Medications
Medications may be prescribed to manage fluid balance in various ways.
- Diuretics promote fluid excretion and are used to treat fluid overload or edema.
- Electrolyte supplements are used to correct electrolyte imbalances.
- Vasodilators are used to improve blood flow and reduce fluid retention.
- Antidiuretic hormone (ADH) is used to reduce urine output and prevent dehydration.
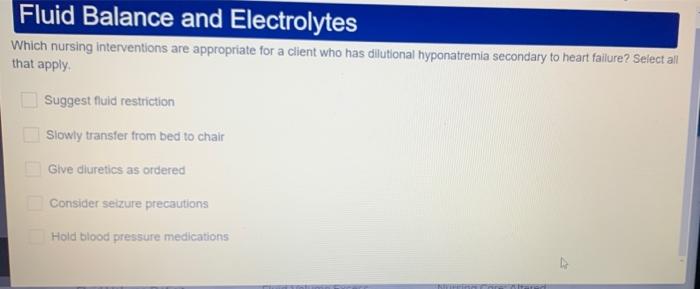
Nursing Interventions
Nursing interventions play a crucial role in managing fluid balance in patients. They encompass monitoring, education, and collaboration to ensure optimal patient outcomes.
Monitoring
Monitoring the patient’s fluid status is essential to assess fluid balance and detect any deviations from normal. This involves:
- Regular assessment of vital signs, including blood pressure, heart rate, and respiratory rate, to detect signs of dehydration or fluid overload.
- Daily monitoring of weight and fluid intake and output to track fluid balance and identify any imbalances.
- Assessment of skin turgor, mucous membranes, and capillary refill time to evaluate hydration status.
Education
Patient education is vital for promoting self-care and maintaining fluid balance. Nurses provide education on:
- The importance of fluid balance and its role in maintaining overall health.
- Signs and symptoms of dehydration and fluid overload, and when to seek medical attention.
- Appropriate fluid intake recommendations based on individual needs and activity level.
- Strategies for staying hydrated, such as drinking plenty of fluids throughout the day and avoiding excessive caffeine and alcohol.
Collaboration
Nurses collaborate with other healthcare professionals to manage fluid balance in patients. This includes:
- Consulting with physicians to determine appropriate fluid intake and output goals.
- Working with dietitians to provide nutritional guidance and ensure adequate electrolyte intake.
- Collaborating with pharmacists to monitor fluid-related medications and their potential side effects.
Questions and Answers
What are the key indicators of fluid imbalance?
Changes in vital signs, such as heart rate, blood pressure, and respiratory rate, as well as alterations in urine output, skin turgor, and mental status.
How is fluid balance managed in patients?
Through careful monitoring of fluid intake and output, administration of intravenous fluids or electrolytes as needed, and adjustment of medications that affect fluid balance.